If your hemoglobin (Hb) is low, you might feel worn out, light-headed, or short of breath. The good news: many cases improve with smart food choices, better absorption habits, and—when needed—well-guided supplements. This guide explains exactly how to raise hemoglobin in a safe, science-based way. It’s written in plain English, with quick-scan tables so you can act right away.
Quick note: Low hemoglobin can have many causes. Food is powerful, but it isn’t a cure-all. If your Hb is low, work with a clinician to find the cause and a plan that fits you. See the “When to see a doctor” section for red flags.
What is Hemoglobin and Why It Drops
Hemoglobin is the oxygen-carrying protein in red blood cells. Without enough Hb, your tissues don’t get the oxygen they need—so you feel tired, weak, and breathless. Iron deficiency is the most common global cause of anemia, but vitamin B12 and folate (B9) shortages, chronic disease, blood loss (heavy periods, GI bleeding), kidney disease, and certain medicines can also lower Hb.
Normal Hb Ranges (Adults)
Normal ranges vary by lab, altitude, and health status. Below are typical adult values used in many labs, plus WHO anemia cut-offs. Use your lab’s reference range to interpret your test.
| Group | Typical lab range (g/dL)* | WHO anemia threshold (g/dL) |
|---|---|---|
| Adult men | ~13.5–17.5 | <13.0 |
| Adult women (non-pregnant) | ~12.0–15.5 | <12.0 |
| Pregnant women | — | <11.0 (varies by trimester) |
*Ranges differ by lab; your report will show the correct reference. WHO anemia cutoffs are widely used in public health.
Step 1: Know Your Cause (and Check the Right Labs)
Before you try to fix low Hb, find the cause. Doctors often order a CBC (complete blood count) and iron studies:
- Ferritin — reflects iron stores; the first test to confirm iron deficiency. It can be falsely high during inflammation, so clinicians may also check CRP.
- Transferrin saturation (TSAT) and serum iron — help show how much iron is available.
- B12 and folate — rule out megaloblastic anemia (enlarged red cells due to vitamin shortage).
- If you’re male or post-menopausal (or have GI symptoms), guidelines often call for a GI evaluation to look for bleeding or malabsorption.
At-a-glance: tests and what they mean
| Test | What it suggests | Why it matters |
|---|---|---|
| Ferritin | Low ferritin = low iron stores | Best first marker of iron deficiency (with clinical context) |
| TSAT | Low % = poor iron availability | Helps decide if oral or IV iron needed |
| B12 & folate | Low = megaloblastic anemia | You must treat the right deficiency |
| CRP | High = inflammation | Can mask low ferritin |
| Stool/Endoscopy (selected adults) | Finds GI blood loss | Common hidden cause of iron deficiency |
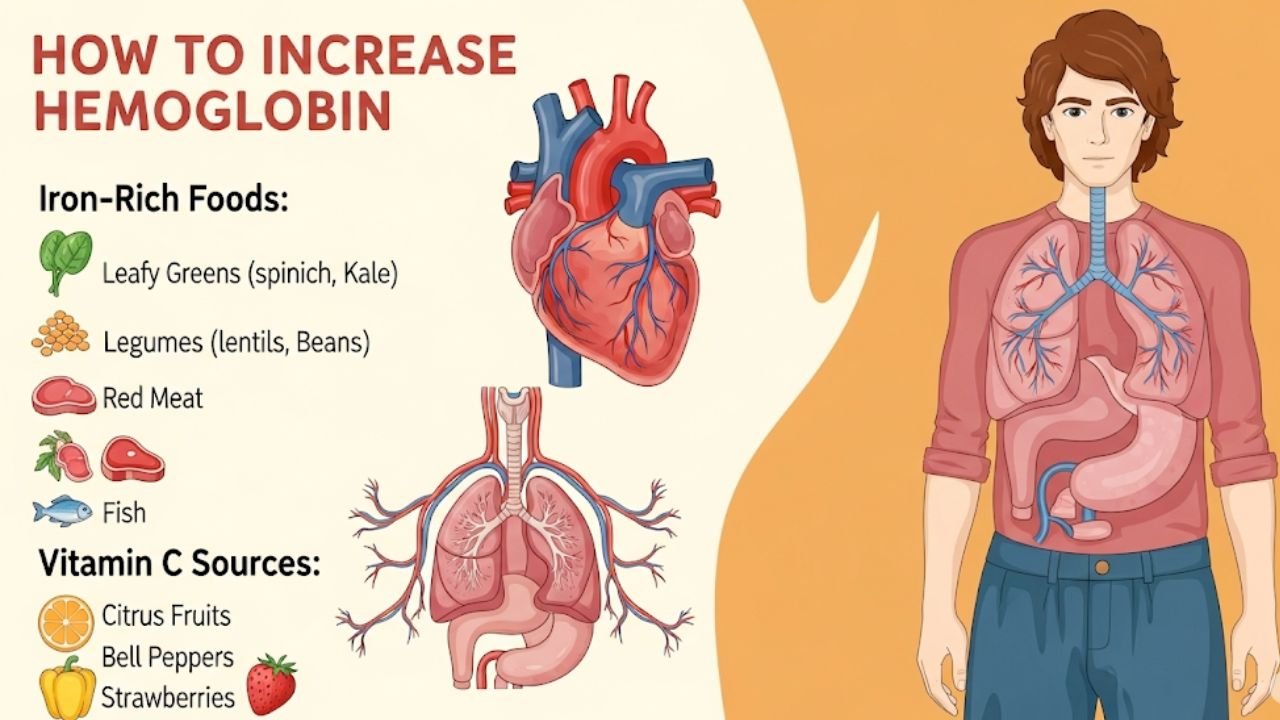
Step 2: Build an Iron-Smart Plate
You can nudge hemoglobin up with iron-rich foods plus absorption boosters (and by avoiding things that block iron around meals).
The Two Types of Dietary Iron
- Heme iron (from animal foods) is absorbed more easily.
- Non-heme iron (from plants and fortified foods) is absorbed less efficiently—but you can boost it with vitamin C and by pairing with meat/fish/poultry.
Iron-Rich Foods (per standard portion)
Use this list to plan meals. Portions follow U.S. Dietary Guidelines tables but the foods are global—mix and match with your cuisine.
| Food (heme unless noted) | Portion | Iron (mg) |
|---|---|---|
| Oysters | 3 oysters | 6.9 |
| Mussels | 3 oz (85 g) | 5.7 |
| Beef (various cuts) | 3 oz (85 g) | ~2.5 |
| Sardines, canned | 3 oz (85 g) | 2.5 |
| Clams | 3 oz (85 g) | 2.4 |
| Lamb | 3 oz (85 g) | 2.0 |
| Fortified ready-to-eat cereal (varies by brand) | ½–1 cup | 9.0–16.2 |
| Hot wheat cereal, fortified | 1 cup | 12.8 |
| Spinach, cooked (non-heme) | 1 cup | 6.4 |
| White beans, cooked (non-heme) | ½ cup | 3.3 |
| Lentils, cooked (non-heme) | ½ cup | 3.3 |
| Soybeans, cooked (non-heme) | ½ cup | 4.4 |
| Jerusalem artichoke, cooked (non-heme) | 1 cup | 5.1 |
| Prune juice, 100% (non-heme) | 1 cup | 3.0 |
Numbers from U.S. Dietary Guidelines food-source tables (compiled from USDA FoodData Central). Actual iron varies by brand/variety.
Smart Pairings to Absorb More
- Add vitamin C (citrus, guava, amla, peppers, tomatoes) to plant-iron meals. Ascorbic acid can markedly increase non-heme iron absorption.
- Include a little meat/fish/poultry with beans or greens; the “meat factor” also boosts absorption.
At-a-glance: high-absorption meal ideas
| Meal | Why it works |
|---|---|
| Chana masala with tomatoes + squeeze of lemon | Non-heme iron + vitamin C enhancer |
| Dal with sautéed spinach + side of grilled fish | Plant iron + “meat factor” |
| Fortified oats topped with strawberries/kiwi | Fortification + vitamin C |
| Whole-grain wrap with hummus + bell peppers | Plant iron + vitamin C |
What Blocks Iron (time it right)
Some foods and drinks are fine—just don’t take them with your iron-rich meal:
- Tea and coffee polyphenols can cut non-heme iron absorption (classic studies show ~40–70% with a meal; leaving a 1-hour gap helps).
- Calcium (large doses from supplements or dairy) may reduce iron absorption; many experts suggest taking calcium and iron at different times.
- Phytates in bran/legumes and some polyphenol-rich foods can inhibit non-heme iron—vitamin C helps counter this.
At-a-glance: timing tips
| Item | Keep away from iron-rich meals by… |
|---|---|
| Tea/coffee | ~1 hour (before or after) to reduce the block |
| Calcium supplements | Separate from iron by several hours |
| High-fiber bran cereal | Don’t pair with your iron pill |
Step 3: Use Fortification and Kitchen Tricks
- Fortified cereals/grains can deliver big iron in small portions (check the label for %DV).
- Cast-iron cookware can increase the iron in acidic, moist foods (like tomato-based dishes), though the amount varies by food and pan. It’s a helpful extra, not a cure on its own.
At-a-glance: easy wins
| Trick | How to try it |
|---|---|
| Choose a cereal with ≥50–100% DV iron per serving | Pair with fruit rich in vitamin C |
| Cook dal/beans with tomato or lemon | Boosts absorption |
| Use a well-seasoned cast-iron pan for sauces/chillis | Adds a little extra iron (varies) |
Step 4: Consider Iron Supplements (the right way)
Supplements are powerful—and not always gentle. Use them under medical advice, after confirming the cause.
What to know before starting
- Forms: Common options are ferrous sulfate, ferrous gluconate, ferrous fumarate; “elemental iron” content differs by form. Some newer forms (e.g., polysaccharide iron) may be gentler.
- Side effects: Nausea, constipation, dark stools are common with higher doses.
- Timing: Many clinicians suggest taking iron on an empty stomach or with vitamin C if tolerated. Avoid taking with tea/coffee or calcium.
Daily vs. Alternate-Day Dosing
Recent research shows high single doses can raise hepcidin, a hormone that temporarily blocks absorption—so back-to-back high doses may be less efficient. In some studies, alternate-day dosing improved fractional absorption and may be better tolerated; whether it’s clinically better for everyone is still being studied. Ask your clinician which plan fits your case.
At-a-glance: supplement basics
| Topic | Key point |
|---|---|
| Confirm deficiency | Check ferritin/TSAT before starting |
| Elemental iron | Check the label; forms differ in % elemental iron |
| Dosing pattern | Daily or alternate-day—individualize with your clinician |
| Interactions | Separate from calcium; watch meds like levothyroxine, PPIs (ask your doctor/pharmacist) |
Step 5: How Fast Will Hemoglobin Rise?
With effective iron therapy (and the cause addressed), Hb often rises ~1 g/dL (10 g/L) within about 2 weeks, with steady gains over 4–8 weeks. You typically continue iron for 3 months after Hb normalizes to refill stores. Your doctor will set the exact timeline and follow-up tests.
At-a-glance: check-up plan (example—your clinician may differ)
| Time | What to check | Why |
|---|---|---|
| 2–4 weeks after starting iron | Hb, symptoms | Expect a rise if therapy is working |
| 8–12 weeks | Hb + ferritin | Confirm correction and repletion |
| After normalization | Keep iron 3 more months (if prescribed) | Rebuild stores to prevent relapse |
Step 6: Special Situations
Pregnancy
Iron needs rise in pregnancy; many women take a prenatal with iron. Low Hb in pregnancy needs careful evaluation and treatment to support mother and baby. Always follow your obstetrician’s plan.
At-a-glance: pregnancy notes
| Topic | Why it matters |
|---|---|
| Higher iron needs | Blood volume expands; fetus/placenta need iron |
| Prenatal iron | Often recommended; dosing individualized |
| Avoid DIY dosing | Balance benefits vs. side effects with your OB |
Vegetarians and Vegans
Plant-based diets are healthy but non-heme iron is less bioavailable. The iron RDA for vegetarians is ~1.8× higher to account for this. Focus on legumes, tofu/tempeh, seeds, greens, fortified grains—plus vitamin C at meals.
At-a-glance: plant-based iron gameplan
| Do this | Examples |
|---|---|
| Choose rich sources daily | Lentils, chickpeas, soy, pumpkin/sesame seeds |
| Use fortification | Breakfast cereals, flours (check labels) |
| Add vitamin C | Citrus, amla, bell peppers, tomatoes |
| Watch blockers | Time tea/coffee away from meals |
Frequent Blood Donors
Each whole-blood donation removes ~200–250 mg of iron. Young and frequent donors often need low-dose iron for ~60 days post-donation (per U.S. Red Cross/AABB guidance). Ask your blood center or clinician for a plan.
At-a-glance: donor recovery
| Action | Typical guidance* |
|---|---|
| Low-dose iron | 18–38 mg elemental iron daily for ~60 days after whole-blood donation |
| Diet focus | Iron-rich + vitamin C foods |
| Ferritin testing | Consider if you donate often |
*General guidance from donor organizations; confirm locally.
When Oral Iron Isn’t Enough
If you can’t tolerate pills, have severe deficiency, inflammatory bowel disease, chronic kidney disease, or ongoing blood loss, your clinician may suggest IV iron and investigate the underlying cause. GI evaluation is especially important in adult men and post-menopausal women with iron deficiency anemia.
Symptom Relief and Everyday Habits
Small daily habits help while Hb is climbing:
- Spread iron across meals. Include at least one iron-rich item at each meal.
- Hydrate and move. Gentle activity and hydration can ease fatigue while you recover.
- Avoid smoking. Smoking impacts oxygen delivery and overall health.
When to See a Doctor (Don’t Wait on These)
Call your clinician promptly if you have:
- Severe fatigue, fainting, chest pain, palpitations, or shortness of breath, especially at rest.
- Very heavy periods, black/tarry stools, or visible blood in stool.
- Neurologic symptoms (numbness/tingling) that could suggest B12 deficiency.
- No improvement after several weeks of correct iron therapy.
These can signal serious anemia or another condition that needs urgent care.
At-a-glance: red flags
| Symptom | Why it matters |
|---|---|
| Chest pain/shortness of breath | Can signal severe anemia/heart strain |
| Black/tarry stools | Possible GI bleeding |
| Rapid heartbeat, dizziness, fainting | Low oxygen delivery |
| Numbness/tingling | Possible B12-related nerve issues |
Sample 7-Day “Increase Hemoglobin” Menu Ideas (Mix & Match)
Use these as inspiration; adjust portions to your needs, culture, and preferences.
| Day | Breakfast | Lunch | Dinner | Snack |
|---|---|---|---|---|
| 1 | Fortified oats + strawberries | Chana masala + lemon | Grilled fish + sautéed spinach | Handful of roasted chickpeas |
| 2 | Egg + whole-grain toast + tomato | Lentil soup + side salad | Beef/lamb stir-fry + peppers | Prune juice (small glass) |
| 3 | Fortified cereal + kiwi | Tofu bhurji + chapati | Dal + mustard greens | Orange + pumpkin seeds |
| 4 | Yogurt (separate from iron meal) + berries | Bean salad + citrus vinaigrette | Mussels/clams with tomato | Hummus + bell pepper |
| 5 | Besan chilla + chutney | Rajma + brown rice + lemon | Sardines + mixed veg | Guava |
| 6 | Poha with peanuts + lime | Chickpea wrap + spinach | Chicken/lamb + broccoli | Dates (2–3) |
| 7 | Upma + tomato | Lentil khichdi + lemon | Oysters or tofu + greens | Small fortified cereal snack |
(Keep tea/coffee at least an hour away from iron-rich meals to improve absorption.)
FAQ: Quick Answers
How long until I feel better?
Many people feel more energetic within 2–4 weeks of effective treatment; full correction and re-filling iron stores takes longer. Stick with follow-ups.
Can I just take vitamin C instead of iron?
No. Vitamin C helps absorb non-heme iron; it doesn’t replace iron.
Is spinach enough?
Spinach has iron, but it also has inhibitors. Pair with vitamin C and other sources (beans, fortified cereal, seafood, meat).
Is too much iron harmful?
Yes. Avoid high-dose iron unless prescribed. Keep iron supplements away from children; accidental overdose can be deadly.
Strong Conclusion
Raising hemoglobin is a two-part job: replenish iron (and other missing nutrients), and fix the cause. Build iron-smart meals, time tea/coffee and calcium away from those meals, and use supplements only when tests—and your clinician—say they’re needed. Track your progress with follow-up labs. With steady steps, most people can restore healthy Hb and feel their energy return.